[adinserter block=”5″]
Demodex mites in rosacea – it’s confirmed by scientific information [5] that Demodex mites play an important role in rosacea! Anyone with rosacea knows how frustrating the condition is and how few good treatment options there are to sustain a remission. I’ve long been treating my rosacea patients by combining medicines and skin care recommendations to help heal rosacea prone skin and prevent reoccurance by ‘covering all the bases’ we know play a role in rosacea – including addressing mites.
Knowledge is power. This guide helps you to gain control of rosacea and the notorious Demodex mites. We look into treatment plans, the best routines and most effective products, and the very nature of these pesky microscopic foes. You’ll be equipped to successfully conquer facial mites and facial redness, skin sensitivity, rosacea bumps, and achieve a radiant, healthy complexion.
Scientists Have Been Rethinking the Significance of Mites in Rosacea!
Researchers continue to unravel the complex relationship between Demodex mites and rosacea.
We’ve long known that:
- Every person has Demodex mites in their skin pores (yes, it’s unsavory but true).
- People with rosacea have even more mites in their pores than normal.
Because everybody has Demodex mites, tiny creatures that live naturally in our pores, doctors have ignored their presence. I haven’t. Over many years, I’d see mite stuffed pores under the microscope as an incidental finding on skin biopsies. I’d noted that it often correlated with run-away rosacea [6] including pustules, red sensitive skin, and often patches of skin with small spikes of whitish scale sticking out of facial pores that were surrounded by redness (pityriasis folliculorum). Because of this, I’ve been treating Demodex mites for decades and found that my rosacea patient’s skin improves when I do!
I’m thrilled that recent scientific studies are giving us some interesting information that supports my treatment methods.
Results of more and more scientific papers are suggesting a significant role for Demodex mites in driving rosacea of both facial skin and the eyes. In fact, authors of a scientific review paper [7] on rosacea and Demodex say this about the role of Demodex in rosacea:
“Rosacea favors the proliferation of Demodex, and the over-proliferation of Demodex aggravates the symptoms of rosacea, thus forming a vicious circle.”
We look deeper into the relationship between mites and rosacea, including causes, bacteria on mites, skin problems, eyelash mites, mites on scalps, and other facts below. But first let’s look at your Demodex mites and rosacea treatment options:
What is the Treatment for Demodex Mites and Rosacea
The care guidelines for rosacea are constantly evolving. In the 35+ years that I’ve practiced dermatology, the standard rosacea therapies have relied on oral and topical antibiotics. We don’t know entirely why antibiotics helped rosacea. It may be by targeting bacteria that are present in the skin or on the mites. Some antibiotics also have anti–inflammatory effects separate from their antibacterial properties.
Many of my patients are unwilling to use antibiotics long term so I’ve worked hard to find alternative treatments – including addressing mites.
Dr. Bailey’s Skin Care Strategy
Science and Decades of Experience Backed Ingredients and Method
I developed my recommendations based on what worked for my many rosacea patients and observations I made under the microscope on skin biopsies. When I have a suspicion that mites are playing a role in a patient’s rosacea symptoms, my strategy includes two key components:
- I include specific topical anti-mite prescription medicines (more on this below)
- Because mite re-infestation is the norm, I also recommend specific skin care steps and products to discourage mites from coming back and thriving in abundance
The approach works synergistically to eliminate and control Demodex mites, soothe inflammation, and reveal a healthier, calmer complexion.
4-Step Skin Care Routine to Treat Rosacea and Demodex Mites
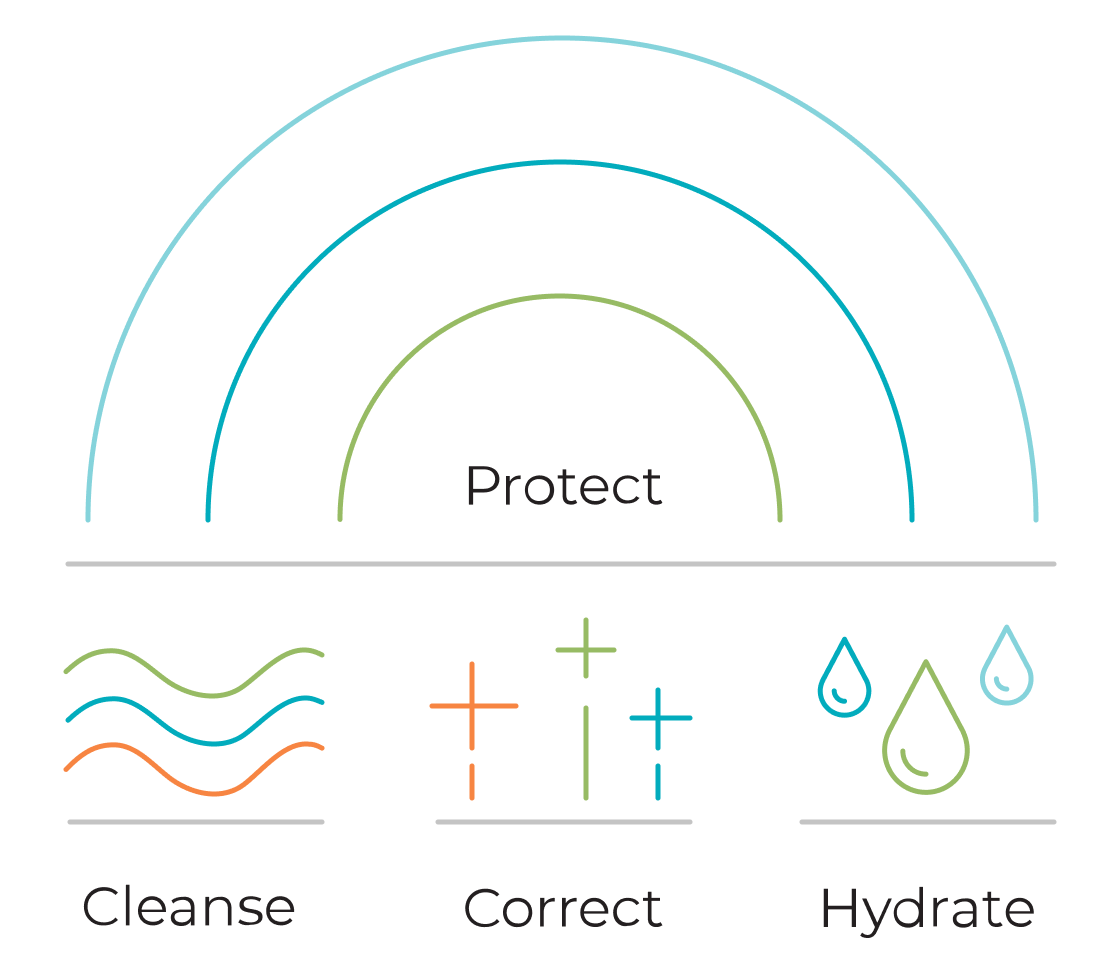
Take control of rosacea and pesky Demodex mites with my Complete Skin Care Routine™ which consists of 4 essential steps: Cleanse, Correct, Hydrate, Protect. As a dermatologist, I’ve seen its transformative power firsthand.
This routine tackles both rosacea and its mitey culprits, leaving you with a calmer, clearer complexion, free from redness, bumps, and breakouts. Your skin will feel soothed, with minimized pores and reflect a healthy, radiant glow.
Remember, consistency and expert guidance are key for optimal results!
The core of this routine is my Rosacea Therapy Kit, and I’ve strategically added the Benzoyl Peroxide Cream and Omega Enriched Face Booster Oil to treat Demodex mites with rosacea.
Let’s look at how to use and layer these products with the 4-step routine:
1. Cleanse
Surface cleansing can wash off Demodex mites outside the pores, along with skin yeast. Facial skin cleansing twice daily is important for controlling Demodex mites. [12]
- Cleanse skin with a 2% pyrithione zinc fortified soap (Calming Zinc) twice a day.
- This helps balance a skin yeast germ called Pityrosporum/Malassezia that also grows abundantly on rosacea-prone complexions.
- Sensitive complexions do best alternating the 2% Calming Zinc soap in the morning with pH balanced soapless Extremely Gentle Foaming Facial Cleanser at night.
- For non-allergic patients, I may choose a prescription skin cleanser with sulfa drugs if necessary.
Always rinse skin really well after cleansing because retained cleanser will irritate skin and continue to pull skin lipids out of skin layers.
2. Correct
Successfully treating facial mites and rosacea isn’t just about cleansing away mites, bacteria, yeast and impurities such as dead skin cells and excess sebum. Science has unlocked a treasure trove of targeted corrective ingredients and potent treatments, waiting to be combined and layered into a personalized routine that unleashes their true potential.
- To correct out of balance skin inflammation, I always have my patients apply Green Tea Antioxidant Skin Therapy first, right after the cleansing and towel drying the skin.
- This soothing cream contains pharmaceutically pure and stable green tea polyphenols equivalent to what is extracted in 500 cups of green tea.
- This popular topical product loads the skin’s antioxidant reserve to help fight skin stressors.
- For oily pustular rosacea and inflammation, try applying Benzoyl Peroxide Cream twice a day to active areas. It can be irritating but can often also be very uniquely appropriate and can possibly address mites.
- If topical medicines are being used, such as metronidazolel, Finacea or ivermectin/Soolantra (which specifically kills Demodex mites), I have my patients layer those on top of the Green Tea cream.
Pro-tip: I prescribe the very economical permethrin cream to my rosacea patients and have them use it on their face and neck twice a day for a week and then twice a day for 1 to 2 days every month to control Demodex mites. This is a unique treatment that I developed so ask your dermatologist if this might be right for you.
3. Hydrate
The hydrate step is important because barrier integrity is weak in rosacea-prone skin. Your skin won’t heal if it is not properly hydrated.
- Hydrate your skin with Daily Moisturizing Face Cream applied over the products you used above.
- Enrich the Daily Moisturizing Face Cream with a few drops of the Omega Enriched Face Booster Oil to benefit from the essential oils (such as sea buckthorn) and castor seed oil.
- At night, you may even want to replace the Moisturizing Cream with the Omega Oil. directly to your face.
4. Protect
The protect step is really important for controlling rosacea because UV exposure can trigger rosacea flares. My top choice for daily sun protection for rosacea prone complexions is a mineral zinc oxide broad spectrum sunscreen.
- Apply the non-irritating Sheer Strength Physical Matte Tinted SPF 50+ Sunscreen during the day – every day – to prevent UV triggering of rosacea.
- It is lightly tinted with iron oxide to help hide complexion flaws. It blends in well to all complexion skin tones, including really fair skin.
- Men love it too because it does NOT look like makeup.
- The matte texture helps hide oily shine.
- The iron oxide helps filter visible and blue screen light known to cause skin damage.
It’s that simple! This non-prescription dermatologist’s Complete Skin Care Routine covers all of the main factors that cause rosacea, trigger rosacea, or are the consequences of rosacea, complete with targeted products that control Demodex mites. If necessary, I combine these targeted skin care products with topical prescription medicines to treat rosacea.
Follow the 4-Step Routine with the Rosacea Therapy Kit
I created my Rosacea Therapy Kit to take the guesswork out of building a healing skin care routine for those suffering from rosacea. The above steps add in the Benzoyl Peroxide Cream and Omega Enriched Face Booster Oil to effectively fight demodex mites with rosacea.
If you already have a pH balanced cleanser (used in step 1) and an SPF (used in step 4) that you love, my Facial Flaking and Redness Solution Kit combine the key non-prescription products I use to target driving factors behind rosacea inflammation.
How the Routine Works
This carefully curated selection of compatible products works together to heal rosacea, boost your skin’s resilience against inflammation and mite overgrowth, and ultimately support sustained remission. For a temperamental condition like rosacea, this comprehensive approach delivers the best possible results.
This routine:
- Fights inflammation with antioxidants from green tea
- Includes ingredients that may fight mites and bacteria such as benzoyl peroxide, castor seed oil and sea buckthorn
- Incorporates zinc pyrithione to fight skin yeast that we have long known contribute to facial redness from rosacea
- Supports the fragile skin barrier to heal with a lipid replenishing facial moisturizer
- Prevents UV ray exposure that can trigger rosacea using a non-irritating zinc oxide sunscreen

NAVIGATE TO KEY SECTIONS OF THIS GUIDE:
Medical Treatments Used by Dermatologists to Treat Demodex Mites in Rosacea
How I’ve Been Treating Facial Demodex Mites in Rosacea Patients
Here, I list some of the Demodex mites treatment options I go over with my rosacea patients. It is important to discuss these with your treating physician to see if they are right for you.

- Oral ivermectin. The mites may come back easily, so repeated treatments over time may be necessary to control Demodex. Oral treatment will penetrate both skin and the eyelash area.
- Topical ivermectin creams, such as Soolantra can treat demodex mites. This can not be used in the eye area. It tends to be an expensive medicine, unfortunately.
- Treatment with permethrin (an off-label approach for Demodex) prescription cream nightly for a week. I have my patients repeat this as necessary. This also can not be used to treat the eye area.
- Topical metronidazole may reduce skin inflammation. Oral metronidazole may have some efficacy against mites though I prefer to rely on topical medicines to treat rosacea.
- IPL (intense pulsed light) also helps reduce the mite population [4]. It also diminishes the blood vessel capillaries and, in my experience, helps reduce skin inflammation in rosacea.
- Natural options include tea tree oil, peppermint oil, salvia oil, bergoment oil, black seed oil and castor seed oil. Of these, I have used castor seed oil in my Omega Enriched Face Oil. All the others are known skin irritants – something we want to avoid in rosacea – and can cause skin allergy.
- Hygiene steps to discourage mite reinfection and overgrowth include keeping skin clean, frequent washing of linens including bed linens, avoiding sharing makeup and facial sponges.
- Following my proven Complete Skin Care Routine for a successful treatment. See the details and steps in the 4-Step Skin Care Routine section of this guide.
My Rosacea Therapy Kit is the core of a skin care routine that supports prescription care so that your rosacea heals. To address Demodex mites, my 4-step skin care routine adds in Benzoyl Peroxide Cream and Omega Enriched Face Booster Oil. (Of course, discuss your skin care routine with your prescribing doctor if you are receiving prescription medicines.)
What Kills Demodex Mites?
Does Benzoyl Peroxide Kill Demodex Mites?
Years ago, I attended an American Academy of Dermatology lecture given by a physician practicing in Israel where they use benzoyl peroxide for Demodex. Permethrin was not available there and topical ivermectin had yet to be invented. This physician said she achieved good control of facial Demodex infestation and rosacea pustules with topical benzoyl peroxide.
Benzoyl peroxide is used in the veterinary medical literature to help control Demodex skin infestations in dogs. In addition, the benzoyl peroxide-erythromycin topical medicine combination has been found beneficial for treating facial demodex infestation in humans. [13]
Benzoyl peroxide can be irritating to sensitive rosacea-prone skin however. I use my alcohol-free Benzoyl Peroxide Cream for complexions suffering from rosacea. Follow the 4-step skin care routine in this guide to incorporate it into your regimen.
Another option is Foaming Benzoyl Peroxide Cleanser. This gentle pH balanced cleanser has a full 10% benzoyl peroxide. Sensitive skin rosacea-prone complexions may not tolerate benzoyl peroxide so care must be taken.
Do Antibiotics Kill Demodex?
No, antibiotics are not antiparasitic medicines. But topical and oral antibiotics have been the mainstay of rosacea therapy for years. They may help reduce mite numbers, slow the return of mites, target the bacteria on the mites that play a role in rosacea and may exert anti-inflammatory effects on rosacea inflamed skin.
Is there a Natural Treatment for Demodex Mites?
Some essential oils appear to kill Demodex mites but at the concentrations used, these oils would be irritating to rosacea. Tea tree, sage, and peppermint were the most effective in a small study [3], though all oils ultimately killed Demodex including sea buckthorn, which is a soothing oil that helps calm skin inflammation.
My Omega Enriched Face Booster Oil (used in step 3 of my skincare routine) incorporates sea buckthorn and castor seed oil, both of which have been studied against Demodex, with other botanical healing oils such as borage, kakui nut, argan oil, pomegranate oil, cypress and others to sooth and support sensitive skin.
I think there is a role for daily botanical oil use to help control the Demodex mite recolonization of rosacea-prone skin. I personally apply my Omega Oil at bedtime on top of my other nighttime treatment products. My 4-step skin care routine guides you on how to use this oil in your rosacea treatment.
Does Pyrithione Zinc Kill Demodex Mites?
Zinc pyrithione in my Calming Zinc Soap (used in step 1 of the routine) has been helpful for controlling rosacea. Whether it helps slow down mites, or their bacteria, or is just working on Pityrosporum/Malassezia yeast, it’s not fully understood, but it is effective and I always recommend it. A Russian study done in 2012 showed that pyrithione zinc reduced both Malassezia skin yeast and demodex mites in patients with seborrheic dermatitis. Seborrhea and rosacea often overlap, as does this yeast and the mites.
Follow the skin care routine above, which incorporates this Zinc Soap with other complimentary products to help fight rosacea and Demodex mites.
NAVIGATE TO KEY SECTIONS OF THIS GUIDE:
The Relationship Between Facial Mites and Rosacea
Do Demodex Mites in the Pores Cause Rosacea?
The pores on your skin are home to many microscopic inhabitants including bacteria, yeast, and – yes – mites. The rosacea puzzle is taking form and microscopic Demodex mites play an important role in the skin problems of rosacea! [1] Mammals, including humans, have Demodex on their skin. Demodex mites primarily live in our pores and oil glands.
Demodex mites:
- Prefer the oiliest parts of our face such as the “T-zone”.
- Eat dead skin cells and sebum (skin oil).
- Are shy! The mites rarely venture out of the pores where they live, lay their eggs, and die.
Exactly how mites cause rosacea is complex and still being worked out. We know that Demodex mites can weaken skin barrier integrity. This leads to excessive skin sensitivity to classic rosacea triggers such as harsh weather, skin care products and even sun.
Some of the early signs of rosacea, including flushing, redness and ‘broken capillaries’ [5], also occur when there are increased numbers of mites in the pores. The red skin bumps of rosacea, called granulomas, happen when skin immune cells collect around mite filled pores.
Studies also suggest that the overgrowth of Demodex mites may eventually alter the skin’s immune balance and capillary function in ways that favor the mite’s own survival and proliferation. [5] As if the mite-skin interaction isn’t complicated enough, additional papers suggests that it’s not just the mites, it’s a protein on a bacteria [8] that the mites carry that causes some of the inflammation of rosacea – wow, you can see how this topic is complicated – and the mite/bacteria/rosacea connection may be one of the reasons why antibiotics have been one of the helpful medicines used to treat rosacea for many years!
What Rosacea Skin Problems are Linked to Demodex Mites?
- Skin barrier fragility (sensitive skin)
- Flushing
- Permanent “broken” facial capillaries
- Sebaceous hyperplasia (enlargement of oil glands)
- The red rash, bumps and pustules of rosacea
People with Rosacea Have More Mites in Their Pores
While we’ve known that rosacea prone complexions have a greater number of mites in the pores, the exact relationship remained a mystery for years. The connection between Demodex mites and rosacea is becoming increasingly clear. Demodex mites are capable of trigger an inflammatory cascade that leads to the symptoms of rosacea. Scientific studies in medical journals have also gathered evidence on how bacteria living on human Demodex mites may play a crucial role in triggering a complex cascade of events that lead to the skin problems of rosacea flares.
Many scientific papers now link the skin problems characteristic of rosacea such as redness, bumps, excessive skin sensitivity, flushing and increased visible skin capillaries with Demodex mites. This knowledge paves the way for potentially more effective and personalized treatment options in the future.
Please see my proven 4-step system in this guide that combines my Rosacea Therapy Kit with the mite-fighting duo of Benzoyl Peroxide Cream and Omega Enriched Face Booster Oil to actively target and eliminate Demodex mites and rosacea.
Bacteria on Demodex Mites May Be the Cause of Rosacea Skin Problems
There are two bacteria that may be to blame, Bacillus oleronius and Staphylococcus epidermidis. Interestingly, these microbes are sensitive to the antibiotics that we dermatologists have used for years to treat rosacea. It may have been the mite’s bacteria that we’ve been treating all along. Conclusions haven’t been reached but it’s fascinating, surprising, and just a little creepy. I discuss my approach to medical treatments in the above section.
Eyelash Mites: People with Rosacea Have More Demodex Mites in Their Eyelash Follicles
Having rosacea means that you are more likely to have an increased number of mites [9] in the hair follicles of your eyelashes. Demodex mites in eyelash hair follicles can result in blepharitis with redness, swelling and itching of the skin along the lash line. Dandruff [10] of the lashline with buildup of scale and crusting has also been linked to the presence of Demodex. It is possible to have these eyelash symptoms with or without occular rosacea.
See the Medical Treatments I use to treat Demodex mites in eyelashes.
Demodex Mites Can Cause Pustules, Redness, and Scale on the Scalp
Demodex in the hair follicles of the scalp can be associated with some of the same symptoms of rosacea, namely redness and pustules. [11] That said, this does not mean that having rosacea on your face means that you have rosacea on your scalp. It does mean that if you have a lot of mites in the pores of your face and lash line, you may also have mites in the follicles of the scalp. The good news is that some of the oral mite treatments (see my treatment approach above) that help control the mites driving your rosacea may also address mites along the lashline and in the hair follicles of your scalp.
NAVIGATE TO KEY SECTIONS OF THIS GUIDE:
The Facts About Demodex Mites on Our Skin and Eyelashes
Demodex mites live in the pores on places of the human body where there is a lot of oil (T-zone, chest, ear canal, and groin). Only rarely can they get through the lining of the pore and into the second layer of the skin called the dermis. When they do, they may cause severe inflammation such as large inflammatory pustules (pimples). It may be this entrance into the skin that is responsible for some of the worst inflammatory aspects of rosacea.
- Demodex mites live for less than 3 weeks and their eggs hatch in less than 3 days.
- They have to be in a pore to survive; they can’t live outside the pore. They only come out of the pore at night to mate, traveling at most ½ inch away from their home for dating purposes! When done, they scramble back down into their pore to lay their eggs.
- Human babies are born with no mites, and then their pores slowly become inhabited by them. Every race in all parts of the world has Demodex mites – sorry to break the news but none of us are spared!
- As we age, we become more likely to have a lot of mites in our pores. In fact, 100% of the elderly have Demodex mites in their pores. It may be the quality of sebum (oil) not the quantity that makes the pores hospitable for the mites since the elderly outpace teens in skin mite density. There may also be some element of immune underperformance on the part of our skin that allows the mites to thrive.
- There are two types of mites; they live in different parts of the pores and cause different manifestations of rosacea.
- Demodex folliculorum lives in the main portion of the pore and it’s more likely to cause scaling redness and sensitive skin.
- Demodex brevis lives deeper in the sebaceous glands (which comes off the pore) and is more likely to cause the papulopustular eruption (rosacea pimples), the symmetrical rashes, and other skin problems arising on the background of a pre-existing rosacea.
- The B. oleronius bacteria are found on the Demodex mites that colonize human skin. It may actually be a protein on the B. oleronius bacterium that is capable of leading to some of the important inflammatory cascade seen in rosacea including ocular rosacea.
- Demodex can act as a vector for bacteria and the mites presence is associated with co-infecting skin bacteria and fungi. This co-infection may play a role in skin problems such as chalazions, styes, pustules and red bumps among others.
The Bottom Line with Mites and Rosacea
The bottom line is that we may be getting closer to understanding Demodex mites and rosacea. I expect to see more targeted treatments being developed, and maybe even a cure, as the research continues. For now, the new focus on mites is gross, but fascinating. As a final note the authors of a study [1] state:
The pathogenic role of Demodex mites, as well as B. oleronius and S. epidermidis, in the induction and persistence of rosacea remains an unresolved issue.
So, until then, we patients and physicians have to be creative at trying to reign in the inflammation and skin problems of rosacea.
Take Control of Rosacea and Demodex Mites
As a dermatologist, I’ve seen the frustration of persistent rosacea and Demodex flare-ups. The 4-step skin care routine outlined in this guide combines the power of the hand-selected products in my Rosacea Therapy Kit with the scientifically-backed benefits of Omega Enriched Face Oil and Benzoyl Peroxide Cream.
This consistent approach with a targeted attack on both rosacea and Demodex mites helped me heal many of my patience with lasting results.
By building your routine with these potent allies, layering them for maximum impact, you’ll unlock the door to a radiant, even-toned complexion. Your skin can be free from redness, irritation, and pesky bumps and resilient against everyday stressors, both environmental and microscopic.
Explore Further
If you would like a more in-depth discussion on rosacea skin care, check out the following guides:
Download a Free Copy of My Rosacea eBook
Learn all about what it is and what you can do about it.
Other articles you can learn more from:
You can also visit my Skin Care Advice page and scroll down to the Glossary where you will find a listing of my most popular rosacea articles.
NAVIGATE TO KEY SECTIONS OF THIS GUIDE:
About the Author
Dr. Cynthia Bailey M.D. is a Board Certified dermatologist practicing dermatology since 1987. She has done well over 200,000 skin exams during her career and authors the longest running physician written skin health blog in the world.
References
- The potential role of Demodex folliculorum mites and bacteria in the induction of rosacea. Stanisław Jarmuda, Niamh O’Reilly, Ryszard Żaba, Oliwia Jakubowicz, Andrzej Szkaradkiewicz and Kevin Kavanagh Journal of Medical Microbiology Papers in Press . Published August 29, 2012
- Treatment of demodicosis in dogs: 2011 clinical practice guidelines. Ralf S Mueller, Emmanuel Bensignor, Lluís Ferrer, Birgit Holm, Stephen Lemarie, Manon Paradis, Michael A Shipstone. National Center for Biotechnology Information, February 13, 2012
- Effect of essential oils on the survival rate of Demodex spp. Maciej K Oseka; Aleksandra Sedzikowska, iOVS Avro Journal, April 2014
- Dispelling the Mystery of Demodex, The Dermatologist, January 2007
- Forton FMN. The Pathogenic Role of Demodex Mites in Rosacea: A Potential Therapeutic Target Already in Erythematotelangiectatic Rosacea? Dermatol Ther (Heidelb). 2020 Dec;10(6):1229-1253. doi: 10.1007/s13555-020-00458-9. Epub 2020 Oct 23. PMID: 33095403; PMCID: PMC7649190.
- Forton F, Germaux MA, Brasseur T, De Liever A, Laporte M, Mathys C, Sass U, Stene JJ, Thibaut S, Tytgat M, Seys B. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005 Jan;52(1):74-87. doi: 10.1016/j.jaad.2004.05.034. PMID: 15627084, PubMed
- Fen Wei, Li Li, Yi Kong, Xiaofeng Yan, Kevin J. Varghese, Song Zhang, Jian Jiang, Bao Chai, Hongxiang Chen; Evidence for the Clinical Association between Demodex and Rosacea: A Review. Dermatology 2023; Karger
- Two AM, Wu W, Gallo RL, Hata TR. Rosacea: part I. Introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015 May;72(5):749-58; quiz 759-60. doi: 10.1016/j.jaad.2014.08.028. PMID: 25890455, PubMed
- Gonzalez-Hinojosa D, Jaime-Villalonga A, Aguilar-Montes G, Lammoglia-Ordiales L. Demodex and rosacea: Is there a relationship? Indian J Ophthalmol. 2018 Jan;66(1):36-38. doi: 10.4103/ijo.IJO_514_17. PMID: 29283119; PMCID: PMC5778578 PubMed
- Cheng, A.M., Galor, A., Banoub, R. et al. The impact of ocular demodicosis on the eyes. Eye 37, 3061–3062 (2023).
- Helou W, Avitan-Hersh E, Bergman R. Demodex Folliculitis of the Scalp: Clinicopathological Study of an Uncommon Entity. Am J Dermatopathol. 2016 Sep;38(9):658-63. doi: 10.1097/DAD.0000000000000512. PMID: 26959693. PubMed
- Chudzicka-Strugała I, Gołębiewska I, Brudecki G, Elamin W, Zwoździak B. Demodicosis in Different Age Groups and Alternative Treatment Options-A Review. J Clin Med. 2023 Feb 19;12(4):1649. doi: 10.3390/jcm12041649. PMID: 36836184; PMCID: PMC9961532. MDPI
- Oztürkcan S, Ermertcan AT, Sahin MT, Afşar FS. Efficiency of benzoyl peroxide-erythromycin gel in comparison with metronidazole gel in the treatment of acne rosacea. J Dermatol. 2004 Aug;31(8):610-7. doi: 10.1111/j.1346-8138.2004.tb00566.x. PMID: 15492433; PubMed
Additional Studies Referenced
Zhao YE, Wu LP et. al., Retrospective analysis of the association between Demodex infestation and rosacea, Arch Dermatol. 2010 Aug;146(8):896-902
Elston DM, Demodex mites: facts and controversies, Clin Dermatol. 2010 Sept-Oct;28(5):502-4
Li J, O’Reilly N, et. al., Correlation between ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in patients with facial rosacea, Ophthalmology. 2010 May;117(5):870-877
Gao YY, Di Pascuale MA, In vitro and in vivo killing of ocular Demodex by tea tree oil, Br J Ophthalmol 2005 Nov;89(11);1468-73
Forton FM. Papulopustular rosacea, skin immunity and Demodex: pityriasis folliculorum as a missing link. J Eur Acad Dermatol Venereol. 2012 Jan;26(1):19-28. doi: 10.1111/j.1468-3083.2011.04310.x. Epub 2011 Oct 24. PMID: 22017468.
Kim JS, Seo BH, Cha DR, Suh HS, Choi YS. Maintenance of Remission after Oral Metronidazole Add-on Therapy in Rosacea Treatment: A Retrospective, Comparative Study. Ann Dermatol. 2022 Dec;34(6):451-460. doi: 10.5021/ad.22.093. PMID: 36478427; PMCID: PMC9763916.
MOKRONOSOVA M.A., GLUSHAKOVA A.M., GOLYSHEVA E.V., ZHELTIKOVA T.M. Demodex mites and Malassezia yeast at patients with seborrheic dermatitis // Vestnik dermatologii i venerologii. – 2012. – Vol. 88. – N. 3. – P. 92-98. doi: 10.25208/vdv693
[adinserter block=”5″]
Source link




